Cervical Lordosis and Bruxism: What Your Pain Is Telling You
What If Your Neck and Jaw Pain Were Connected?
Have you ever felt a dull ache at the base of your skull or along your jawline and wondered if it was just stress or bad posture? What if those annoying twinges in your neck and the headaches that follow aren’t just random—but connected to how you hold your head and how tightly you clench your teeth?
It turns out there’s a strong and often-overlooked link between the curve of your neck—known as cervical lordosis—and the unconscious habit of jaw clenching or teeth grinding, a condition known as bruxism. While these two issues are usually treated separately—by dentists for bruxism and chiropractors or physical therapists for posture—clinical observations and emerging research suggest that they may actually feed into one another.
Cervical lordosis is the natural inward curve of your neck that helps support the weight of your head and maintain healthy alignment of your spine. When this curve flattens or shifts, often due to forward head posture or chronic tension, it disrupts the delicate balance of muscles and nerves running from your neck to your face. At the same time, bruxism places constant strain on the jaw, TMJ, and upper cervical spine—exacerbating any underlying issues.
Understanding this connection isn’t just interesting—it’s empowering. By recognizing the patterns that contribute to your symptoms, you can seek care that actually addresses the root cause instead of just masking the pain. Whether through pain journaling, biofeedback tools like ClenchAlert, or posture correction, uncovering the full picture can help you finally feel better—and be heard by the right healthcare professionals.
Understanding Cervical Lordosis: The Neck’s Natural Curve
At the top of your spine, just beneath your skull, lies a gentle inward curve known as cervical lordosis. This curve is not a flaw—it’s a vital feature of your body’s structural blueprint. It helps distribute the weight of your head evenly over your shoulders and spine, allowing you to stand upright, move your neck freely, and protect delicate nerve pathways that connect your brain to the rest of your body.
But when this natural curve starts to flatten, exaggerate, or reverse, problems can arise. This change in posture is known as a loss of cervical lordosis or hypolordosis. It often develops gradually—especially in people who spend long hours sitting, looking down at screens, or holding tension in their shoulders. Over time, this misalignment strains the muscles and ligaments of the neck, compresses nerves, and disrupts the body’s normal biomechanics.
Common symptoms of cervical lordosis issues include:
- Persistent neck pain or stiffness
- Headaches that start at the base of the skull
- Tingling or numbness in the arms or hands
- Poor balance or visual strain
- Increased tension in the jaw and face
These symptoms can be confusing because they don’t always point to a single cause. And unless someone examines your posture—and how it interacts with your jaw function—they may be dismissed or treated in isolation.
In fact, many people with a straightened neck curve don’t even realize it until they see an X-ray or visit a specialist. But once identified, cervical lordosis becomes an essential piece of the puzzle—especially when it's part of a broader pattern of chronic pain, tension, or bruxism. Recognizing this foundational misalignment helps guide treatment that restores your body's natural balance from the top down.
What Is Bruxism? When Your Teeth Bear the Tension
Bruxism is more than just teeth grinding at night—it’s a complex, often unconscious habit that can wear down your teeth, tighten your jaw muscles, and contribute to widespread pain. It comes in two main forms: awake bruxism, which involves clenching the jaw during the day (often in response to stress or concentration), and sleep bruxism, which typically involves rhythmic or forceful grinding during the night.
While the occasional jaw clench might seem harmless, repeated episodes over time can take a toll. Teeth may flatten or chip, gums may recede, and the jaw joint—called the temporomandibular joint (TMJ)—may become inflamed or misaligned. You might wake up with a sore jaw or find yourself massaging your temples without even realizing why. In some cases, bruxism is so severe it causes headaches, ear pain, or neck stiffness.
The causes of bruxism are multifactorial. Emotional stress, sleep disturbances, medications (such as SSRIs), and even postural habits can all play a role. Some people grind their teeth during REM sleep due to arousals in the nervous system; others may clench during work hours as a coping mechanism for anxiety or tension. But regardless of the root cause, one thing is clear: bruxism is rarely just a dental issue.
What makes bruxism particularly tricky is that it often flies under the radar. Many people don’t realize they clench until their dentist notices wear on their molars or a partner hears grinding at night. By the time symptoms show up—whether as tooth damage, headaches, or TMJ dysfunction—the habit is usually well established.
Bruxism also places enormous pressure on the muscles that connect your jaw to your skull and neck. This tension doesn’t stay localized—it radiates. That’s why people with bruxism often report not only dental symptoms, but also face, neck, and shoulder pain. And when that pressure meets a misaligned cervical spine, the result can be a cycle of chronic discomfort that’s hard to escape—unless both conditions are addressed together.
Bridging the Gap: How Neck Posture Affects Jaw Mechanics
It might seem like your neck and jaw operate in separate systems, but anatomically and neurologically, they’re tightly linked. The posture of your cervical spine directly influences the position of your jaw, the function of your temporomandibular joint (TMJ), and even the behavior of the muscles that control chewing and clenching. When cervical lordosis is compromised—flattened or shifted forward—it can start a chain reaction that makes bruxism more likely, more intense, and harder to treat.
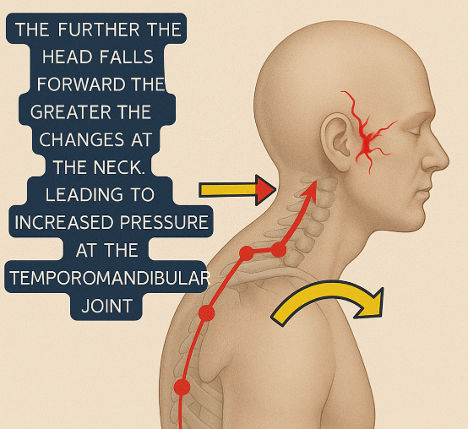
Let’s start with posture. When your head juts forward—often called forward head posture—it increases the mechanical load on the muscles at the back of your neck. These muscles then pull and compensate, affecting the balance and alignment of the entire upper body. As the head shifts out of alignment, the mandible (lower jaw) often moves along with it, altering your bite and the resting position of your jaw. This subtle shift may trigger compensatory muscle activation in the jaw, neck, and shoulders, reinforcing clenching and grinding behaviors.
On the neurological side, the trigeminal nerve, which controls sensation in the face and motor functions like biting and chewing, shares close anatomical connections with the cervical nerves of the upper spine. Compression or irritation of these nerves due to poor neck alignment can lead to heightened muscle tension, altered sensory processing, and pain referral patterns that blur the lines between jaw, head, and neck symptoms.
You might feel jaw tension after working at your computer all day, or notice that your neck feels tighter after a night of heavy clenching. These aren’t coincidences—they’re signs of an integrated system under strain.
Understanding this biomechanical and neurological relationship is critical. If a practitioner only treats the jaw without evaluating cervical alignment, the underlying issue may persist. Likewise, correcting posture without addressing habitual clenching may not fully relieve symptoms. It’s the interplay between these structures—and the way they adapt to stress—that makes the bruxism-cervical lordosis connection so important to investigate.
Pain Journaling: A Critical Tool for Patterns, Triggers, and Clarity
One of the most effective—and most overlooked—tools for managing chronic jaw and neck pain is something simple you can start today: pain journaling. By regularly documenting your symptoms, behaviors, and circumstances, you can begin to see patterns that are otherwise invisible. This awareness is not just empowering—it’s essential for helping your healthcare provider connect the dots between cervical lordosis, bruxism, and related symptoms.
At its core, pain journaling is about capturing the when, where, and why of your pain. Each time you notice discomfort—whether it’s jaw tension, a dull headache, or neck stiffness—write down:
The time of day and location of the pain
The intensity of symptoms (on a 1–10 scale)
What you were doing or thinking about at the time
Your stress level, emotional state, or posture
If you noticed clenching, grinding, or a change in your bite
Any recent activities, like long drives, heavy screen use, or disrupted sleep
Over time, a pattern may emerge. You might realize that your jaw tension worsens during work Zoom calls or that headaches follow nights when you sleep on your stomach. Perhaps certain foods, medications, or emotional triggers contribute to your bruxism episodes. These insights help identify the behavioral, postural, and environmental factors that fuel the feedback loop between your jaw and neck.
Even more importantly, a pain journal gives you something concrete to bring to your clinician. Whether you’re seeing a dentist, chiropractor, or physical therapist, documented patterns allow them to make more targeted evaluations and treatment recommendations. You’ll spend less time guessing and more time healing.
Pain journaling also pairs well with biofeedback devices like ClenchAlert. These tools give you real-time alerts when you're clenching, which you can record alongside your journal notes. This integrated feedback loop allows you to recognize subconscious behaviors and understand how they're linked to posture, stress, and daily activities—making it easier to change them.
Ultimately, journaling transforms you from a passive recipient of care into an active participant in your recovery. And when it comes to complex conditions like cervical lordosis and bruxism, your observations may hold the missing piece of the puzzle.
The Real-Life Symptoms That Leave Patients (and Providers) Stumped
If you’ve ever bounced from doctor to dentist to chiropractor without clear answers for your head, neck, or jaw pain, you’re not alone. Many people with cervical misalignment and bruxism experience a constellation of vague, persistent symptoms that don’t fit neatly into a single diagnosis. And because the symptoms can overlap across different systems—neurological, muscular, and dental—they’re often misdiagnosed, downplayed, or treated in isolation.
One day, it might be a dull earache. The next, a tension headache or tooth sensitivity. You might notice clicking in your jaw when you chew or wake up with a sore neck after what should have been a full night’s sleep. Some days, your shoulders feel tight for no apparent reason. The frustrating part? Each individual symptom might be addressed by a different type of clinician—and still, the root cause remains unresolved.
This fragmented approach is especially common in people with both altered cervical lordosis and undiagnosed bruxism. When the natural neck curve is compromised, the altered posture affects the TMJ and supporting muscles. Meanwhile, habitual clenching—often triggered by stress or compensation for poor alignment—only worsens the tension. The cycle continues, feeding itself day after day.
Complicating matters further is the fact that many of these symptoms are considered “nonspecific” in standard medical evaluations. Jaw clenching may be brushed off as a stress response. Neck pain gets chalked up to a poor pillow or bad sleep. But when viewed through the lens of interconnected systems, these symptoms start to tell a different story.
Recognizing this pattern is a crucial step toward real relief. The key is not to chase each symptom individually, but to view them as part of a broader mechanical and neurological dysfunction. A misaligned neck and an overactive jaw aren’t separate problems—they’re partners in pain. And unless both are addressed together, treatment may fall short.
If this sounds like your experience, don’t be discouraged. You’re not imagining it, and you’re not alone. This blog aims to help you—and your providers—reframe the problem so you can pursue a more effective, integrated approach to healing.
Who Can Help: Building a Collaborative Care Team
When your symptoms straddle the line between dentistry, neurology, musculoskeletal alignment, and behavioral stress, no single specialist can provide a complete solution. That’s why people with cervical lordosis and bruxism often benefit most from a collaborative care approach—where multiple providers work together to uncover and treat the root cause of your symptoms.
So who should be on your care team?
Start with the professional most aligned with your primary complaint. If you're dealing with jaw soreness, tooth wear, or TMJ clicking, a dentist—especially one familiar with temporomandibular disorders (TMD)—is a logical first stop. Dentists can assess occlusion (how your teeth come together), evaluate for signs of grinding or clenching, and offer initial protection via nightguards or splints.
If your posture, neck pain, or mobility are primary concerns, a chiropractor or physical therapist can evaluate the curvature of your cervical spine and any forward head posture. These professionals can use hands-on techniques, corrective exercises, and postural retraining to help restore natural alignment and reduce strain on the muscles that connect your neck and jaw.
If your symptoms include headaches, dizziness, or nerve-related pain, a neurologist or pain specialist might be needed to rule out underlying neurological conditions. In cases where stress and anxiety are clearly contributing to the clenching behavior, a psychologist or behavioral therapist can offer tools for stress reduction and habit modification.
And then there are tools like biofeedback, which fall into a category of their own. A wearable device such as ClenchAlert can enhance your self-awareness and provide real-time feedback when you’re clenching—helping you reinforce good habits like “lips together, teeth apart.” Sharing this data with your provider can further tailor your treatment.
Ultimately, a team-based strategy offers the best chance for lasting relief. Communication between providers—along with your own pain journal and symptom observations—creates a full picture of what’s happening. And that collaborative insight is exactly what’s needed to treat the whole person, not just the individual parts.
Biofeedback: Awareness Is the First Step to Behavior Change
In the quest to relieve jaw and neck pain, there’s a tool that often gets overlooked but can make all the difference: biofeedback. Unlike mouthguards that passively protect the teeth or medications that numb symptoms, biofeedback empowers you to recognize what your body is doing in real time—and then do something about it.
The premise is simple: if you can sense when you’re clenching your jaw, you can learn to stop. But here’s the challenge—many people clench unconsciously, especially during the day when they’re stressed, focused, or distracted. That’s where a device like ClenchAlert comes in.
ClenchAlert is a small, wearable biofeedback dental guard designed for people who struggle with awake bruxism. It fits comfortably over your teeth, just like a traditional mouthguard—but with one critical difference: when you clench, it gently vibrates. That tactile cue alerts you to your behavior so you can relax your jaw, reset your posture, and return to a healthier resting state—lips together, teeth apart.
This feedback loop helps retrain your nervous system. Over time, the goal is to reduce the frequency and intensity of clenching episodes—even when the device isn’t in use. It’s not about punishing behavior; it’s about building awareness. You begin to notice patterns, like clenching during emails or while sitting with poor posture. And when paired with pain journaling, biofeedback becomes a powerful teaching tool: you don’t just learn that you’re clenching—you learn why.
ClenchAlert is designed to be worn during the day, especially during high-stress periods, long work sessions, or whenever you notice your jaw tends to tighten. Some people wear it while commuting or working at a computer, while others integrate it into their evening wind-down routine. Unlike bulky splints or EMG headbands, ClenchAlert is discreet, lightweight, and built for real-world use.
What makes biofeedback so impactful is that it turns your body into your guide. It bridges the gap between subconscious behavior and conscious change. In the context of cervical lordosis and bruxism, that means breaking the feedback loop of muscle tension, poor posture, and pain—one vibration at a time.
Conclusion: You Deserve an Answer, Not Just a Mouthguard
If you’ve been living with persistent jaw tension, neck pain, or fatigue that doesn’t respond to traditional treatment, you may have already encountered the frustrating cycle of partial answers. A dentist may prescribe a nightguard. A chiropractor may adjust your neck. A doctor may order imaging—or dismiss your concerns as stress. Each response offers a piece of the puzzle, but rarely does anyone step back to ask: what’s the full picture?
The truth is, cervical lordosis and bruxism are not isolated conditions. They are often symptoms of a broader neuromuscular imbalance—one that affects the entire head, neck, and jaw system. When your neck loses its natural curve, your head moves forward, increasing the workload on your upper spine and altering the position of your jaw. This postural shift affects the muscles that control chewing, breathing, and head support, often triggering or worsening clenching behavior.
Bruxism, in turn, perpetuates the tension. It places enormous strain on the temporomandibular joint (TMJ) and surrounding muscles, exacerbating inflammation, disrupting sleep, and sending ripple effects throughout your body. And because both cervical misalignment and bruxism are influenced by stress, emotional state, and unconscious behavior, they can become deeply ingrained over time—unless you intervene consciously.
That’s why the most effective path forward isn’t a single intervention—it’s an integrated approach grounded in awareness. And it begins with you.
Start by keeping a pain journal. Write down when symptoms occur, what you were doing or feeling at the time, and how long they last. Over days or weeks, this practice often reveals patterns that even experienced clinicians might miss. Your pain journal becomes a roadmap—not just for understanding your body, but for helping professionals tailor a plan that actually works.
From there, consider tools like ClenchAlert, a wearable biofeedback dental guard designed to interrupt the clenching habit and reinforce healthy jaw posture. Every time you clench, ClenchAlert responds with a gentle vibration, reminding you to relax. It’s not punitive—it’s corrective. And when used during your most tension-filled hours—whether at your desk or during your commute—it can help rewire muscle memory and reduce strain on the jaw and neck.
Pair this with professional guidance. Physical therapists can help restore cervical curvature through targeted stretches and postural retraining. Dentists can ensure your bite is balanced and not contributing to the problem. Behavioral specialists can work with you to manage anxiety and unconscious habits that lead to clenching. And when everyone is working from the same map—your symptom journal, your biofeedback data, and your shared insights—you move from confusion to clarity.
You don’t have to settle for piecemeal care or explanations that don’t quite add up. If you suspect your neck and jaw pain are connected, you’re probably right. And with the right combination of observation, technology, and interdisciplinary care, you can get the answers you’ve been missing—not just a mouthguard, but a plan for lasting relief.
Frequently Asked Questions
1. Can cervical lordosis cause jaw pain or contribute to bruxism?
Yes. When the natural curve of the neck is lost, it alters head and jaw position, increasing strain on the TMJ and surrounding muscles. This misalignment can contribute to clenching and grinding behaviors, especially when paired with stress or poor posture.
2. What are the symptoms of a flattened cervical curve?
Common symptoms include neck stiffness, upper back pain, tension headaches, visual strain, numbness in the arms or fingers, and in some cases, referred pain to the jaw or face.
3. How do I know if I have bruxism if I don’t grind my teeth at night?
Bruxism isn’t limited to nighttime grinding. Daytime clenching (awake bruxism) is extremely common and may show up as jaw soreness, facial tightness, or headaches. Many people are unaware of the habit until they track symptoms or use a biofeedback device like ClenchAlert.
4. What is ClenchAlert and how does it help?
ClenchAlert is a wearable dental guard that detects clenching and vibrates to gently alert the user. This haptic feedback encourages a relaxed jaw posture—lips together, teeth apart—and helps reduce clenching episodes over time through awareness and behavior retraining.
5. Is biofeedback safe to use every day?
Yes. Most biofeedback tools like ClenchAlert are non-invasive and safe for daily use. They are designed to be comfortable and help build self-awareness, not cause discomfort or disrupt sleep.
6. How does pain journaling support diagnosis and treatment?
By documenting when and where symptoms occur, you create a detailed log that reveals patterns over time. This information helps your care team make more accurate diagnoses and tailor treatment to your unique needs.
7. Who should I see if I suspect a link between my jaw pain and posture?
You may benefit from an interdisciplinary approach. Start with a dentist or TMJ specialist if your teeth or jaw are involved, and consult a physical therapist or chiropractor for postural evaluation. Sharing your symptom history with both is key.
8. Can correcting my posture eliminate bruxism?
Posture correction may reduce one contributing factor, but it typically needs to be part of a broader treatment plan that includes stress management, jaw awareness, and sometimes behavioral therapy or oral appliances.
9. Does stress really play that big a role in clenching and grinding?
Yes. Stress and anxiety are major drivers of awake bruxism. Many people clench their jaws when concentrating, under pressure, or emotionally triggered. Addressing these root causes can significantly reduce bruxism.
10. Can ClenchAlert replace a nightguard?
ClenchAlert is intended for awake use, not as a replacement for nighttime dental protection. However, it plays a different role—it teaches awareness and behavioral change. Many users combine ClenchAlert during the day with a passive nightguard at night if needed.